Table of Contents
COPD Explained
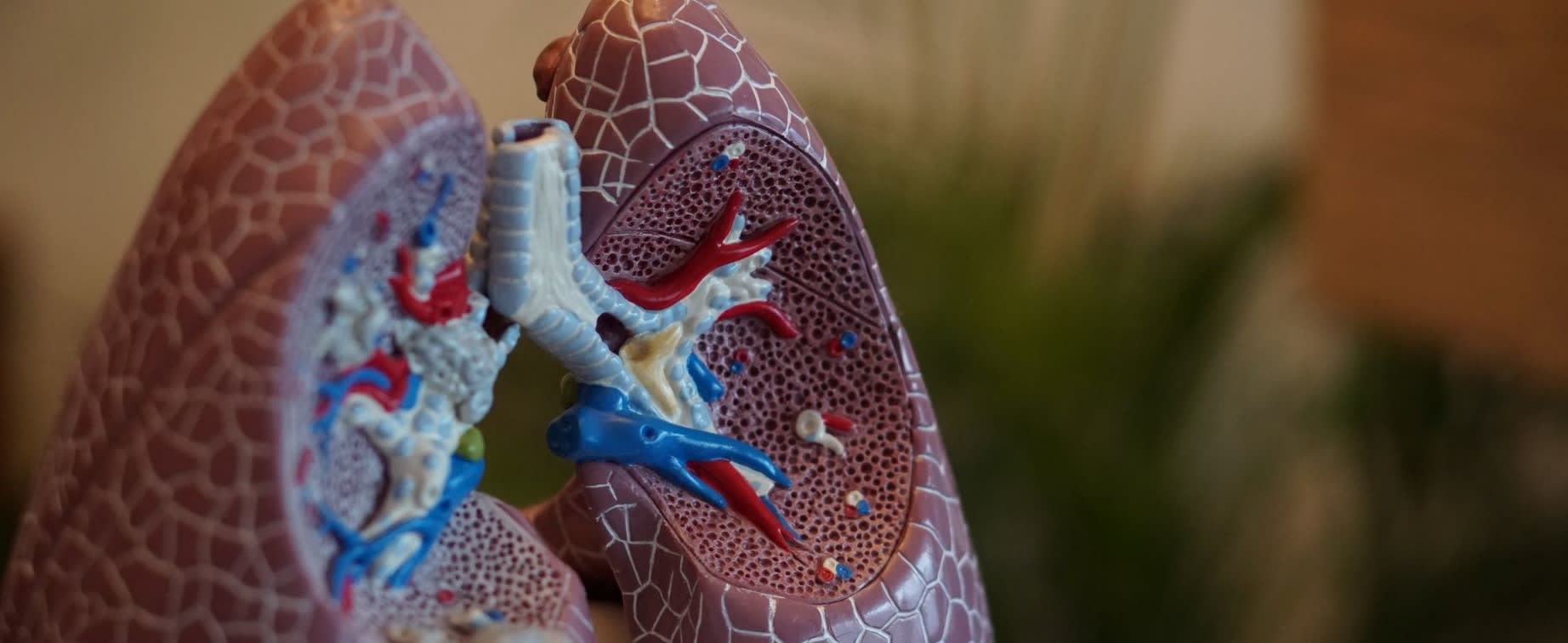
Chronic Obstructive Pulmonary Disease (COPD) is a term that describes a grouping of chronic lung diseases such as chronic bronchitis and emphysema. COPD is currently not curable, but there are many diagnostic, treatment, and management tools available that can help you to breathe with more ease and enjoy life. Some popular inhalers include albuterol (Ventolin) and Atrovent. COPD is characterized by a feeling of breathlessness and sometimes a chronic cough. COPD is a slowly progressing disease and often, people don't realize they have it until it's already severe.
Chronic
Chronic is defined as a disease that persists for a long time and is always present. The symptoms of COPD may take many years to develop, and severity may differ in each person and at different times.
Obstructive
Obstructive is defined as causing deliberate blockages, difficulties, or delays. In COPD, the ability to move air in and out of the lungs, to breathe, is obstructive. Extra mucus, inflammation, and tissue damage can cause these blockages in the airways of the lungs.
Pulmonary
The location of the disease is in the lungs.
Disease
Disease is defined as a disorder in the structure or function of a human. Disease produces signs and symptoms in a specific location. With COPD, the lungs are damaged, causing disease.
Types of COPD
More than 15.3 million people in the US suffer from COPD. In COPD, the airways of the lungs become inflamed, tissue is destroyed, and mucus and damage cause the airways to thicken. Thus, as the airways become obstructed, the flow of air in and out of the lungs decreases, making it harder to breathe. As a result, oxygen is unable to access bodily tissues as it usually does, and causes a buildup of waste gas such as carbon dioxide. Emphysema and bronchitis are the two types of COPD. Most people have symptoms of both bronchitis and emphysema. Therefore health professionals refer to the overarching condition as COPD. [1]
Emphysema
Emphysema is characterized by damage to the air sacs of the lungs, called the alveoli. The alveoli of the lungs may also be narrowed, collapsed, destroyed, stretched, or over-inflated due to COPD emphysema. The inside walls of the alveoli begin to disappear, making these once small sacs to increase in size and become larger. Because of the over-sized alveoli, the larger air sacs do not transfer oxygen between the air and blood as efficiently as they used to. The damage to the alveoli can decrease respiratory function and cause a feeling of shortness of breath. As the alveoli become damaged, the lungs can lose their elasticity as they become overstretched. [2]

Chronic Bronchitis
Chronic bronchitis is caused by inflammation of the bronchial tubes (breathing airways in the lungs) over a long period. The damaged bronchial tubes and inflammation cause excess mucus production, coughing, shortness of breath, frequent infections, and disability. [3]
There are tiny hair-like fibers that lined the bronchial tubes called cilia. In chronic bronchitis, the cilia, which typically helps mucus to move up the tubes and be coughed out, are destroyed. As a result, coughing up mucus becomes more challenging, and the person with this condition ends up coughing even more. If mucus comes up with a cough that has lasted for at least three months, two years in a row, this is considered chronic bronchitis. [2]
Four Stages of COPD
For most people, COPD develops slowly over time. But for other individuals, COPD can progress rapidly. Your doctor is the best person to consult, even if you are experiencing minor symptoms, as they can track your condition over time. Once a diagnosis is given, tracking the stages of COPD can help to modify your treatment plan to best suit your needs over time. Stages of COPD range from mild to severe, and as the stages progress, airflow becomes increasingly limited.
The two common ways to determine COPD stages are the GOLD Staging System or the BODE Index. The Global Initiative for Chronic Obstructive Lung Disease developed the GOLD Staging System. In the GOLD System, a measurement — forced expiratory volume in one second (FEV1) —from a pulmonary function test is used to determine the stage of the COPD in question.
The stages of COPD include:
Stage 1 (mild COPD): Mild COPD with a FEV1 of about 80 percent or higher of the normal range.
Stage 2 (moderate COPD): Moderate COPD with a FEV1 between 50 and 80 percent.
Stage 3 (severe COPD): Severe emphysema with a FEV1 between 30 and 50 percent.
Stage 4 (very severe COPD): Very severe (end-stage) COPD with a FEV1 of 30 percent or lower, or accompanied by low blood oxygen levels at Stage 3. [4]
Symptoms of COPD
Although COPD may not be curable, there are early warning signs that may indicate the onset of COPD. Many people do not recognize the symptoms of the disease until they enter the later stages of its progression. Shortness of breath or a lingering cough could be early warning signs of COPD; if you are experiencing these symptoms or any listed below, always speak with your doctor. Early detection of COPD is beneficial to a successful treatment, so don't wait for symptoms to worsen before you seek professional help.
Early symptoms include:
- Recurrent, mild cough
- Needing to clear your throat often
- Shortness of breath occasionally, especially after exercise
- Symptoms of COPD may include:
- Chronic cough
- Shortness of breath, especially while doing everyday activities
- Frequent respiratory infections
- Wheezing
- Fatigue
- Producing a lot of mucus (phlegm, sputum)
- Blueness of the fingernail beds or lips (cyanosis) [1]
What Causes COPD?
One of the main causes of COPD is the long-term exposure to irritants that damage the lungs and its airways. There are a handful of other known causes for COPD, outlined below.
Smoking
Cigarette smoke is the most common lung irritant in the US responsible for causing 85 to 90 percent of COPD cases. Other forms of smoking, such as pipe, cigar, and various other types of tobacco smoke, can cause COPD. The thousands of chemicals inhaled in cigarette smoking weaken the lungs’ defense against infections, create swelling, narrow air passages, and destroy air sacs, which all contribute to COPD. [1]
The use of e-cigarettes and vaping devices is a more recent occurrence, and more research needs to be done; the use of these devices can cause similar inflammation in the lungs and may be linked with COPD. [5]
Long-term exposure to air pollution, secondhand smoke, dust, chemicals, and fumes can cause COPD. The air that you breathe every day at work, home, and outside can play a role in your COPD diagnosis. Alpha-1 antitrypsin deficiency is a genetic (inherited) condition that affects the body’s ability to protect the lungs from damage. Individuals who are diagnosed with emphysema in their 30s or 40s may have this rare genetic disorder. People with this condition have low blood levels of the alpha-1 antitrypsin (AAT), which is a protein made in the liver. Low levels of AAT can cause lung damage, especially if you are exposed to lung irritants and smoke. Smoking with this condition causes COPD to worsen rapidly. [6] Asthma is a condition where the airways of the lungs narrow, swell and produce extra mucus. Asthma can make breathing difficult and trigger coughing and shortness of breath. Some people with asthma may develop COPD. Treatment options can reverse inflammation and narrowing that are characteristic of asthma, which may prevent COPD in the future. COPD diagnosis is based upon signs and symptoms related to the condition (such as excess mucus production), genetics and family history, and test results. Your doctor will want to know your health history and current health status. Your doctor may ask questions like: A pulmonary function test measures factors such as volume, speed, and function. How fast you can breathe and how much air you can breathe in and out can be measured by this kind of test. Another purpose of the test is to analyze how well the lungs deliver oxygen to the blood. For COPD, the primary type of pulmonary function test used is called spirometry. A spirometry test measures how much air and how fast you can breathe in and out. It is a painless and quick test to take that involves a small machine connected to a tube called a spirometer. Your doctor will instruct you to take a few deep breaths at maximum speed and sometimes involves medicine to measure if it is needed or not. Spirometry tests are highly sensitive and can measure COPD symptoms before they develop. The test results can also measure the severity of your COPD to help you set attainable treatment goals. A spirometry test can also test for asthma or heart failure — other conditions that may be causing your symptoms. The National Heart, Lung, and Blood Institute has an informative video that demonstrates the procedures involved when taking a spirometry lung test. Chest x-ray and CT scans are imaging tests that can provide an in-depth look at the lungs and heart and surrounding tissues. These pictures can show if there are any signs of COPD. Images can determine if another condition, such as heart failure, is responsible for your COPD symptoms. An arterial blood gas test measures the amount of oxygen present in your blood by using a sample taken from an artery. This test shows how well the lungs filter oxygen to the blood and carbon dioxide out of the blood and the body. An arterial blood gas test may determine whether or not oxygen therapy is needed. Treatment for COPD can help to ease symptoms and slow the progression of the disease. There are several different approaches to treatment, depending on the severity of the COPD. Bronchodilators are commonly prescribed as they help to relax the muscles around the airways, which makes breathing easier. Most bronchodilators are taken using an inhaler. Bronchodilators can be short-acting and last for 4-6 hours or long-lasting and last for 12 hours. Sometimes bronchodilators are prescribed alongside inhaled steroid medications, depending on the severity of your condition. Common bronchodilators prescribed for COPD include albuterol (Ventolin), ipratropium (Atrovent HFA), aclidinium (Tudorza), arformoterol (Brovana), and formoterol (Foradil, Perforomist), to name a few. Vaccines may be recommended to lower the risk of contracting other respiratory illnesses such as pneumonia. Classes of medications used to treat COPD may include: If blood oxygen levels become too low, supplemental oxygen may be necessary. Symptoms of low blood oxygen include feeling short of breath, tired, or confused and can cause damage to the body. Oxygen therapy delivers oxygen from tubes that rest in the nose or through a face mask. Depending on the severity of COPD, supplemental oxygen may be necessary at all times or only at certain times. With people who experience severe COPD, oxygen used throughout the day will help them perform simple tasks with fewer symptoms, improve sleep quality, improve energy levels throughout the day, protect organs from damage, and increase life expectancy. [6] Pulmonary rehabilitation programs combine education, exercise training, counseling, and nutrition advice to rebuild strength and lead a more active lifestyle. The American Lung Association has more information regarding the basics of pulmonary rehabilitation. Certain lifestyle changes can provide relief from your COPD symptoms. Lifestyle changes include: There’s no specific diet associated with COPD, but it is always important to stay healthy by being mindful of the food that you consume. The Lung Institute recommends avoiding mucus-forming foods such as red meat, dairy products (milk, cheese, yogurt, butter, ice cream), bananas, eggs, bread, alcoholic beverages, soda, and coffee. Choosing a variety of foods such as vegetables, fruits, legumes, nuts and seeds, and whole grains can provide a nutrient-dense, mucus-reducing diet that will keep your heart, lungs, and body healthy. Try adding these mucus-reducing foods into your diet: Clinical trials are research studies to test how well new medical approaches work in people with the condition in question. Clinical studies aim to find better ways to understand, prevent, diagnose, or treat a disease. If you choose to take part in a clinical trial, you have an opportunity to contribute knowledge about COPD to health professionals. The American Lung Association has more information about clinical trials for COPD To better understand what a clinical trial experience is like from a patient's perspective, watch the video below. Someone with severe COPD who has difficulty breathing at all times may require surgery. Most often, surgery is a last resort for people whose symptoms have not improved with medication and oxygen therapy. Types of surgeries for someone with severe COPD or emphysema may include: In a bullectomy, doctors remove large bullae (air spaces that are created in place of damaged air sacs) from the lungs. Because ballae can become so large that they interfere with breathing, a bullectomy can help to clear the airways and improve breathing ability. In LVRS, damaged tissue is removed from the lungs to improve lung function, ability to breathe, and quality of life. Lung transplants pose many risks, including rejection of the transplanted organ and infection post-surgery. In a lung transplant, your damaged lung is replaced with a donor's healthy lung and is usually only performed in severe cases of COPD. A COPD diagnosis can feel discouraging, but there are many treatment options available to help you live a joyful, active life. Learn more about stress reduction and breathing techniques that can help to alleviate symptoms associated with your COPD (Link to 4 breathing exercises article). The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis or treatment.
Environmental Irritants
Alpha-1 Deficiency
Asthma
Diagnosis
Pulmonary function tests

Spirometry
Chest X-ray or CT scan
Arterial blood gas test
Treatment
Medication
Oxygen Therapy

Pulmonary rehabilitation
Lifestyle Changes
Clinical Trials
Surgery
Bullectomy
Lung volume reduction surgery (LVRS)
Lung transplant